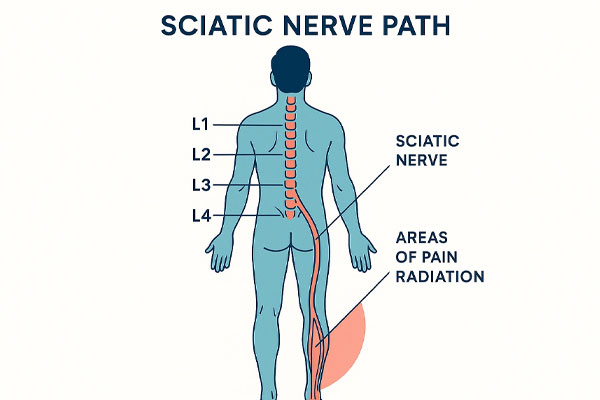
Sciatica is a sharp, radiating pain that often travels from the lower back down to the leg, caused by pressure or irritation of the sciatic nerve. It’s not a disease itself, but a symptom rooted in conditions like a slipped disc, spinal stenosis, or piriformis syndrome. Most patients recover without surgery through a mix of targeted medication, physical therapy, and lifestyle adjustments. Over‑the‑counter anti‑inflammatory drugs, gentle stretching, and alternating cold‑warm compresses help reduce inflammation and relax muscles. In persistent cases, epidural steroid injections or ozone therapy can provide deeper relief without invasive surgery. Maintaining a healthy weight, proper posture, and a nutrient‑rich anti‑inflammatory diet are key to long‑term control. Early diagnosis and active movement, rather than strict rest, accelerate healing. Effective sciatica treatment aims to calm the pain, restore nerve function, and let you reclaim a pain‑free, mobile life.

what will you read…
How Is Sciatica Treated?
Treating sciatica starts with identifying what’s pressing on the sciatic nerve. For most Canadians, non‑surgical care brings lasting relief. Doctors often begin with anti‑inflammatory medications such as ibuprofen or naproxen to calm swelling and reduce pain. Muscle relaxants or nerve‑specific drugs like gabapentin may be added for stubborn discomfort. Once the intense pain settles, physiotherapy and therapeutic massage play a vital role . stretching, gentle soft‑tissue work, core strengthening, and posture training help prevent future flare‑ups. Alternating cold and warm compresses improves blood flow and nerve recovery. In resistant cases, epidural steroid injections deliver direct anti‑inflammatory relief into the spine, while ozone therapy or targeted laser treatment can ease nerve pressure without surgery. Only severe cases with leg weakness or bladder issues require surgical correction such as microdiscectomy. Effective sciatica treatment combines medical precision, movement, massage, and consistent lifestyle changes for true recovery.
Sciatica vs. Regular Back Pain
Many people confuse sciatica with everyday back pain, but the two are worlds apart. Regular back pain tends to stay in one area, often caused by muscle strain, poor posture, or hours of sitting. Sciatica pain travelsit shoots from your lower spine down through the hip and leg, often reaching the toes. That radiating, burning line of pain means the sciatic nerve itself is irritated or compressed, not just the muscles around it. Tingling, numbness, or leg weakness are major red flags that you’re dealing with sciatica, not a simple backache. Unlike general back strain, sciatica usually feels worse when you sit, cough, or twist your body. Recognizing this difference early can save you time, money, and frustration by guiding you straight to nerve‑focused treatment instead of short‑term muscle fixes.
Main Causes of Sciatica Pain
Sciatica pain starts when the long sciatic nerve running from the lower back to the legs gets compressed or inflamed. The most common culprit is a herniated disc, where spinal cushioning slips and presses directly on the nerve. Spinal stenosis is another frequent reason, caused by gradual narrowing of the spinal canal with age or arthritis. Some cases stem from piriformis syndrome, when a small buttock muscle traps the nerve. Less often, spondylolisthesis (vertebral slippage) or injury from falls and heavy lifting can pinch the nerve. Even diabetes may heighten nerve sensitivity. Identifying these causes early ensures precise, non‑surgical treatment that restores mobility and prevents chronic pain.
| Cause | Brief Description | Effect on Sciatic Nerve |
|---|---|---|
| Herniated Disc | Disc bulges or ruptures in the lower spine. | Compresses the nerve root. |
| Spinal Stenosis | Narrowing of the spinal canal. | Reduces space and irritates the nerve. |
| Piriformis Syndrome | Tight buttock muscle near the nerve. | Traps or squeezes the sciatic nerve. |
| Spondylolisthesis | One vertebra slips over another. | Misalignment pinches the nerve. |
| Injury or Trauma | Impact to back or pelvis. | Swelling or pressure on the nerve. |
| Diabetic Neuropathy | Nerve damage from high blood sugar. | Increases nerve sensitivity. |
Non‑Surgical Treatments for Sciatica
Non‑surgical sciatica care focuses on relieving pressure from the inflamed nerve and restoring mobility without the risks of an operating room. The approach combines precise medication, structured physiotherapy, and evidence‑based regenerative procedures. Anti‑inflammatory drugs control immediate pain, while targeted exercises rebuild muscle balance and spinal alignment. When inflammation is severe, minimally invasive options like epidural injections or ozone therapy accelerate recovery. Nutrition and posture correction also support long‑term healing by improving circulation and reducing systemic inflammation. This integrated model.used widely across Canadian pain clinics.offers sustainable relief from recurring sciatica symptoms, helping patients move confidently again without surgery or long recovery downtime.
Targeted Drug Therapy
Targeted drug therapy represents the first line of conservative management for sciatica. Canadian specialists often begin by prescribing non‑steroidal anti‑inflammatory drugs (NSAIDs) to control swelling around the compressed nerve root. For cases complicated by muscle spasm, muscle relaxants such as tizanidine help loosen deep back tissues that irritate the nerve. When patients describe shooting or burning pain down the leg, nerve‑stabilizing medications like gabapentin or pregabalin may be added to quiet abnormal electrical signals. All drugs are adjusted individually to reduce side effects such as drowsiness or gastrointestinal irritation. The goal is relief without dependence. Combined with guided physiotherapy and ergonomic correction, targeted pharmacological care restores functionality, reduces nerve irritation, and forms the foundation for returning to active daily life.
Physiotherapy and Specialized Exercises
Physiotherapy is one of the most reliable non‑surgical solutions for sciatica patients. It rebuilds balance, flexibility, and strength in spinal muscles while easing pressure on the sciatic pathway. Under professional supervision, dynamic stretches such as Cat Cow and Bridge retrain correct posture and lubricate stiff joints. Controlled motion improves circulation, oxygen flow, and nutrient supply to the affected nerve. Each session is personalized to avoid overstress while encouraging healthy spinal alignment. Patients who follow these programs notice reduced pain, better mobility, and improved endurance in just a few weeks. When combined with anti‑inflammatory habits and proper sitting or sleeping posture, physiotherapy works as a powerful long‑term tool to prevent sciatica relapses and chronic muscle fatigue.
Epidural Injection and Ozone Therapy
Epidural steroid injections and ozone therapy offer two minimally invasive alternatives for patients who do not respond fully to medication and exercise alone. An epidural injection delivers a corticosteroid directly into the epidural space of the spine to calm inflammation and relieve pain radiating down the leg. Relief can last for several weeks or even months, providing time to strengthen muscles through physiotherapy. Ozone therapy, popular in advanced pain clinics, introduces a small dose of medical ozone mixed with oxygen to improve tissue healing and reduce oxidative stress. Both methods are outpatient procedures performed under image guidance, requiring no stitches or hospital stay. They effectively close the gap between conservative treatment and surgery, promoting faster recovery and lasting comfort.

Lifestyle Correction
Lifestyle correction completes the holistic plan for sciatica recovery. A balanced anti‑inflammatory diet rich in green vegetables, berries, nuts, and omega‑3 fish helps lower inflammation naturally. Vitamin B12 strengthens nerve sheaths, while magnesium supports healthy muscle contractions and prevents spasms. Hydration, adjusting work ergonomics, and correcting posture reduce daily strain on the lumbar spine. Light activities walking, yoga, or swimming boost blood flow and prevent stiffness. Avoiding prolonged sitting or carrying heavy items helps maintain spinal alignment. When patients commit to these habits, recurrence rates fall dramatically. Lifestyle reform isn’t a quick fix; it’s the foundation for pain‑free motion, improved metabolic health, and long‑term management of sciatica without dependence on constant medication.
Home Remedies for Sciatica
Home treatment for sciatica focuses on reducing inflammation, easing pain, and improving flexibility through natural methods. The foundation is controlled rest, not full bed rest. gentle walking keeps circulation active and prevents stiffness. Applying cold or heat therapy helps manage flare‑ups. Cold reduces acute swelling, while heat relaxes tight muscles and improves blood flow. Gentle stretches like Cat Cow and Bridge open the lower spine, releasing pressure on the nerve. Topical creams containing menthol or capsaicin may provide extra comfort. An anti‑inflammatory diet rich in fish, ginger, and turmeric supports healing from within. Proper sleeping posture. either on your back with a pillow under your knees, or on your side with a cushion between legs. keeps your spine aligned. With patience and discipline, these small daily habits can restore mobility and minimize dependence on painkillers.

When to Use Cold and When to Use Heat?
Knowing when to use cold or heat for sciatica can significantly affect recovery. In the first 48 to 72 hours after a pain flare, cold therapy is best.it constricts blood vessels, decreases swelling, and numbs sharp pain. Use an ice pack wrapped in a towel for 15 to 20 minutes, several times a day. Once acute inflammation subsides, shift to heat therapy. Warm compresses, heating pads, or short warm baths relax spasmed muscles and stimulate oxygen flow to healing tissues. Alternating both can be effective: finish with heat to keep muscles supple. Avoid direct ice or excessive heat to prevent skin burns. This balanced, time‑based approach helps calm nerve irritation faster and supports the body’s natural repair process.crucial for managing long‑term sciatica pain safely at home.
key symptoms
| Symptom | Description | Common Area |
|---|---|---|
| Radiating Pain | Sharp shooting pain from lower back down the leg. | One side, buttock to foot. |
| Numbness / Tingling | Pins‑and‑needles or partial numb feeling. | Calf or outer thigh. |
| Muscle Weakness | Trouble lifting foot or walking normally. | Leg and ankle muscles. |
| Back Stiffness | Tightness or reduced flexibility. | Lower back. |
| Worse When Sitting | Pain increases after sitting too long. | Buttock and thigh. |
| Burning Sensation | Warm, burning pain along nerve path. | Leg or foot. |
When Is Surgery Needed for Sciatica?
Surgery for sciatica is considered only when all conservative methods. like medication, physical therapy, and targeted injections fail to bring lasting relief. Specialists usually recommend surgical evaluation if pain persists beyond six to twelve weeks, or when nerve compression causes muscle weakness, foot drop, or loss of bladder and bowel control. Common procedures include micro discectomy to remove a herniated disc pressing on the sciatic nerve, or laminectomy to widen a narrowed spinal canal. These are minimally invasive in most cases and aim to release trapped nerve roots while protecting spinal stability. Recovery is typically faster today thanks to advanced imaging and refined surgical techniques. Although surgery is rarely the first step, it remains a life‑changing option when sciatica severely limits mobility, daily activity, and quality of life.
Preventing Sciatica Pain from Returning
Long‑term prevention of sciatica pain depends on maintaining spinal health through balanced habits and proper posture. Regular core‑strengthening exercises, such as gentle planks and pelvic tilts, support the lower back and reduce pressure on the sciatic nerve. Avoid sitting for long hours.take short standing or stretching breaks every 30 minutes. Maintain a healthy body weight to minimize spinal stress and choose ergonomic chairs or lumbar cushions when working. A diet rich in omega‑3s, vitamin B complex, and magnesium nourishes nerve tissue and reduces inflammation. Finally, learning correct lifting techniques.bending at the knees, not the waist.prevents reinjury. Consistency in these small daily habits is the most effective safeguard against recurring sciatica episodes and helps sustain pain‑free mobility for the long term.
step by step prevention guide
Strengthen Your Core and Back Muscles
A strong core keeps your spine stable and reduces pressure on the sciatic nerve.
Incorporate gentle routines like bridges, pelvic tilts, and modified planks.
Focus on proper breathing and slow, controlled movement to avoid strain.
Gradual consistency matters more than intensity or duration.
Even five to ten minutes daily help prevent future nerve irritation.
This simple foundation supports a lifetime of spinal resilience.
Maintain Proper Posture Daily
Posture habits directly influence nerve pressure and spinal balance.
When sitting, keep your back straight, shoulders relaxed, and both feet flat.
Avoid bending forward for long periods or twisting your torso suddenly.
Use ergonomic chairs with lumbar support or a small cushion at your lower back.
Regular posture checks reduce chronic tension around the lumbar discs.
Good posture is preventive medicine simple yet highly effective.
Use Safe Movement and Lifting Techniques
Unsafe lifting is one of the quickest ways to trigger sciatica again.
Always bend from your knees, not your waist, and keep objects close to your body.
Move slowly and avoid twisting while carrying weight.
Divide heavy loads and take short breaks between lifts.
Engage your core muscles before each motion to protect spinal joints.
Smart movement means thinking about your back before every action.
Stay Active and Control Body Weight
Light, regular exercise keeps your back mobile and strong.
Activities like walking, swimming, or yoga improve flexibility and blood flow.
Avoid long sitting sessions stand, stretch, or walk every thirty minutes.
A healthy weight prevents extra pressure on lumbar vertebrae.
Consistency in movement helps maintain spinal balance and nerve health.
Active living is the best long‑term defence against recurring pain.
Support Recovery through Nutrition and Rest
Your body heals best when given the right nutrients and recovery time.
Eat foods rich in omega‑3 fatty acids, magnesium, and vitamin B complex.
Stay hydrated to keep spinal discs flexible and properly cushioned.
Prioritise seven to eight hours of quality sleep each night.
Use a supportive mattress that maintains natural spinal alignment.
Rest and nutrition work together to build long‑term resistance to pain.
Frequently Asked Questions About the Best Sciatica Treatment
What are the newest medical breakthroughs in non‑surgical sciatica treatment?
Recent innovations include ultrasound guided steroid injections, nerve‑targeted radiofrequency ablation, and regenerative platelet‑rich plasma (PRP) therapy. These techniques aim to reduce inflammation around the sciatic nerve without surgery. Clinical results show faster recovery and longer‑lasting relief compared with traditional pain‑killer regimens.
How does long‑term sitting at a computer affect the sciatic nerve?
Prolonged sitting, especially with poor posture or crossed legs, compresses the lower spine and tightens gluteal muscles. This can irritate the sciatic nerve pathway. Experts recommend standing breaks every 30 minutes, ergonomic lumbar support, and simple chair stretches to maintain spinal circulation.
Can pregnancy‑related sciatica be treated differently from general sciatica?
Yes, pregnancy‑related sciatica requires gentler, body‑safe approaches. Prenatal yoga, water exercises, and side‑lying sleeping positions relieve discomfort without medication. Applying mild heat and maintaining spinal alignment under professional guidance can safely ease nerve tension for expectant mothers.
What are early warning signs that sciatica may become chronic?
Persistent numbness, tingling beyond six weeks, or leg weakness may signal chronic compression of the sciatic nerve. Ignoring these symptoms can lead to long‑term damage. Early diagnosis, regular physiotherapy, and ergonomic corrections are crucial in preventing chronic nerve irritation.