Best Exercises for Depression and Anxiety are not simply about physical fitness . they represent a form of preventive medicine for the mind. Regular physical activity boosts serotonin and endorphin levels, improves sleep, and reduces cortisol, the body’s main stress hormone. Scientific research confirms that movement therapy like walking, yoga, tai chi, and aerobic workouts enhance mood regulation, sharpen focus, and strengthen emotional resilience. In clinical settings, exercise complements antidepressant therapy by improving motivation and self‑esteem. Even brief daily sessions of about 30 minutes can lift mood as effectively as some medications. For Canadians facing the pressures of modern life, exercise remains an accessible, side‑effect‑free way to restore balance between body and mind. Whether practiced in a gym, a park, or at home, movement reconnects individuals to their sense of control and calm. In short, exercise is not just fitness; it’s mental recovery in motion.
what will you read…
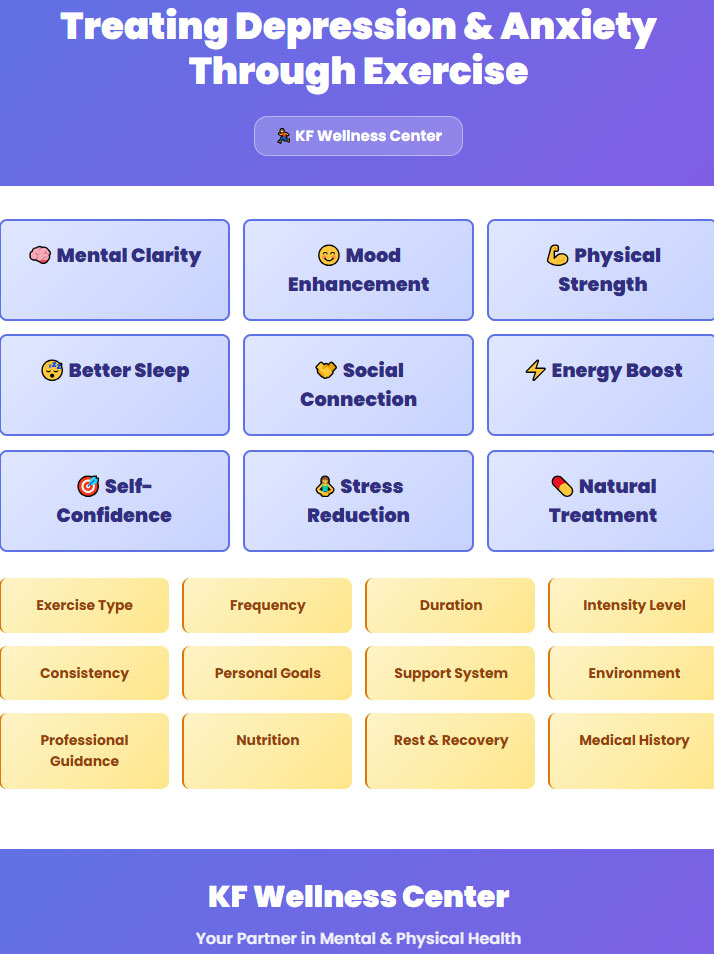
How Exercise Heals the Mind
Exercise acts like therapy for the brain. When you move whether it’s a simple walk, a cardio session, or even a soothing massage at kfwellnesscenter your body releases endorphins and serotonin, the natural mood boosters that lift energy and calm anxious thoughts. At the same time, exercise lowers levels of cortisol, the stress hormone that fuels worry and tension. Better blood flow sends more oxygen to the brain, sharpening focus and improving sleep. Over time, regular movement strengthens areas of the brain that manage emotions, helping people react less to stress and recover faster from low moods. This is why doctors now see exercise and therapeutic massage as key parts of mental‑health care. They are safe, low cost, and effective natural antidepressants that help you feel stronger, think clearer, and regain control of your life.
| Exercise | Psychological Effect | Physical Mechanism | Frequency |
|---|---|---|---|
| Yoga | Calms mind, improves control | Boosts serotonin, lowers cortisol | Daily |
| Walking | Eases tension, clears thoughts | Releases endorphins, improves sleep | 4–5×/week |
| Tai Chi | Builds focus, inner balance | Improves vagal tone, lowers BP | 2–3×/week |
| Aerobic | Lifts mood, increases energy | Raises dopamine, reduces inflammation | 3–4×/week |
| Group Sports | Enhances connection, confidence | Releases oxytocin, reduces isolation | 1–2×/week |
Effective Exercises
Different forms of movement influence mental health in unique ways. The right activity depends on lifestyle, personality, and emotional needs. While gentle disciplines calm the mind, dynamic workouts release energy and reduce internal pressure. From mindful yoga to social team sports, exercise becomes a bridge between body awareness and emotional stability. Each type supports brain chemistry, confidence, and daily motivation powerful allies in managing depression and anxiety.
“Exercise is an all‑natural treatment to fight depression, proving as effective as antidepressant medication for some people.
health.harvard
Yoga
Yoga works as a mind‑body prescription that strengthens both emotional and physical balance. When you step on the mat, each slow pose and deep breath activates a calming circuit in the nervous system. Blood pressure drops, cortisol levels decrease, and the mind becomes lighter. Modern clinics in Canada recommend yoga as a safe complementary treatment for mild depression and anxiety. The combination of breathing and posture teaches self‑control . a core therapeutic goal in cognitive therapy. Scientific research links regular yoga sessions with elevated serotonin and GABA levels, both essential for stable mood. Unlike most workouts, yoga invites mindfulness; it transforms movement into meditation, helping people reconnect with their bodies, accept limitations, and regain internal peace. Twenty minutes a day can genuinely reset how the mind responds to everyday stress.

Walking
Walking remains the most accessible form of natural therapy for emotional recovery. Beyond improving circulation, it stimulates endorphins that ease tension and sadness. Psychologists describe walking as a moving meditation . every step quiets intrusive thoughts while reconnecting the mind with the environment. In Canadian studies, adults who walked outdoors at least five times per week reported reduced anxiety and deeper nightly sleep compared to those exercising indoors. The rhythmic motion of walking, especially in green areas or near water, builds emotional stability and focus. It is also cost‑free and inclusive, fitting all age groups and health levels. For clients struggling with mild depression, structured walking programs gradually rebuild self‑discipline, self‑worth, and daily rhythm. What seems simple becomes powerful: a steady, repetitive movement that heals both the body and the mind.
Tai Chi
Tai Chi is an ancient Chinese discipline blending gentle motion and controlled breathing. It trains mental stillness through physical grace. Each circular move releases muscle tension and synchronizes communication between body and brain. Clinical observations show that patients with chronic anxiety who practise Tai Chi twice a week improve attention, balance, and internal calm. The exercise enhances vagal tone, supporting better heart‑rate variability and emotional resilience. Its slow rhythm offers rest to those who dislike intense workouts yet seek meaningful psychological results. Canadian therapists often integrate Tai Chi into holistic recovery plans for trauma and depression because it combines physical engagement with meditative awareness. Over time, participants describe a growing sense of clarity and grounding. a strong, centered feeling that remains even after the class ends.
Aerobic Workouts
Aerobic workouts like swimming, running, and cycling have a scientifically proven antidepressant effect. Their rhythmic intensity activates circulation, increases neurotransmitter release, and reduces inflammation. a biological factor linked with depression. When heart rate rises moderately, the brain produces dopamine and endorphins that promote optimism and mental clarity. Researchers in Toronto found that thirty minutes of aerobic activity, four times a week, equals the impact of some antidepressants for moderate depression cases. Beyond chemistry, aerobic routines restore routine, sleep quality, and day‑to‑day motivation. For many clients, structured training schedules provide predictability .something often missing in emotional disorders. Aerobic workouts do not just burn calories; they stabilize the mind and enhance self‑efficacy, reminding individuals that active movement can truly rewrite their emotional experience.
Group Sports
Group sports combine exercise, teamwork, and social connection a triad vital for recovery from isolation and low mood. Participating in soccer, tennis doubles, or group fitness creates accountability and shared achievement, triggering the release of oxytocin and serotonin. These hormones reinforce belonging and trust, reducing loneliness, which strongly correlates with depression risk. In Canada, community‑based sport programs have become part of preventive mental‑health strategies because they naturally rebuild motivation and hope. Moreover, friendly competition stimulates focus and teaches emotional regulation under pressure . essential skills for coping with anxiety. Group sports deliver benefits that solo workouts cannot: they combine physical effort with genuine human contact. Over time, participants regain confidence, laugh more easily, and rebuild supportive relationships that last far beyond the field or court.
Training Program
A well‑structured training program is the cornerstone of using exercise as therapy for mental health. Random activity rarely delivers consistent results; what matters is rhythm, progression, and awareness. Every program should begin with a medical check‑up to ensure safety, especially for patients under medication or with cardiovascular conditions. The ideal routine combines warm‑up, main activity, and cool‑down.each phase serving a specific psychological purpose. Warm‑up reduces physiological stress, the main session builds emotional resilience, and cool‑down trains mindfulness and body awareness. Canadian clinical guidelines recommend at least one hundred and fifty minutes of moderate physical activity per week, spread across three to five days. Mixing individual and social exercises prevents monotony and enhances motivation. Tracking mood and sleep patterns along the way helps therapists adjust intensity. A personalized plan transforms movement into an intentional path toward inner balance.
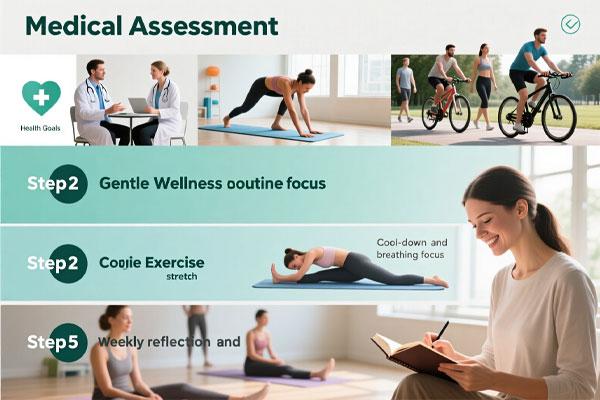
Step by Step Exercise Program
Medical Assessment and Goal Setting
Before any movement, assess both physical and emotional condition. A short consultation with a doctor or therapist ensures safety and realistic expectations. Define clear, measurable goals such as “reduce anxiety attacks” or “improve sleep quality.” Document current medication, mood score, and fitness baseline. This clarity prevents overtraining and improves commitment throughout the process.
Gentle Warm‑Up
Start every session with ten minutes of slow body activation. Combine gentle stretching, shoulder rolls, and deep breathing to awaken muscles and calm the mind. Breathing deeply through the diaphragm reduces cortisol and stimulates body awareness. Focus on how each muscle responds rather than performance. This prepares both the nervous system and the mindset for balanced effort.
Core Exercise Routine
Choose one main activity walking, yoga, cycling, or a light aerobic session and sustain it for 25 to 35 minutes. Keep the intensity moderate: conversation should still be possible. The goal is steady heart engagement without physical exhaustion. Monitor your mood before and after; emotional stability matters more than calorie burn. Over weeks, the body associates movement with calm reward rather than pressure.
Cool‑Down
End each workout with five to ten minutes of light stretching and slow breathing. Lower the heart rate gradually to avoid sudden fatigue. Notice body warmth, heartbeat, and sense of release. Cool‑down phases anchor mindfulness and signal completion to the brain . a small but powerful sense of achievement. This step turns physical effort into emotional reflection.
Weekly Reflection
At the end of each week, take time to evaluate physical energy, sleep patterns, and emotional state. Record observations in a simple journal. If motivation drops or fatigue rises, reduce intensity instead of quitting. Celebrate consistency rather than perfection. Gradual, mindful adaptation keeps the training program sustainable and supports long‑term mental balance.
Medical Considerations
Exercise is often portrayed as a universal remedy, but clinical evidence shows its effects can differ widely depending on an individual’s physical conditions and medication use. Before recommending exercise as therapy for anxiety or depression, healthcare professionals must review cardiovascular status, metabolic conditions, and psychiatric background. An integrated approach.where a therapist, physician, and trainer collaborate.reduces risk and maximizes mental health benefit. The brain.body connection is complex; hormones, neurotransmitters, and circulation interact differently under stress or medication. Proper medical supervision ensures safe intensity levels, timely monitoring, and gradual adjustment. Exercise should never replace prescribed treatment but complement it thoughtfully. A structured, personalized plan transforms physical activity into a therapeutic tool rather than a stressor, allowing patients to feel empowered rather than pressured during recovery.
| Category | Main Concern | Safe Approach | Tip |
|---|---|---|---|
| Medication | Drug–exercise interaction | Moderate effort, spaced from dosage | Track mood and side effects |
| Heart Condition | Risk of over‑strain | Gentle aerobic activity, supervised | Monitor pulse regularly |
| Work Anxiety | High cortisol from stress | Short daily walks, mindfulness | Keep fixed exercise time |
| General Care | Balance of mind and body | Gradual adjustment weekly | Combine therapy and movement |
Integration with Medication
Many individuals managing depression or anxiety rely on antidepressants or mood regulators. Exercise must be integrated carefully to complement not conflict with these prescriptions. Physical activity can influence serotonin and dopamine levels, sometimes mimicking drug effects. This synergy can enhance recovery, but abrupt intensity increases may amplify dizziness, fatigue, or blood pressure fluctuations. Collaboration between physician and trainer is critical for balancing timing and dosage. Ideally, workouts occur several hours after medication intake to allow stable absorption. By monitoring mood and sleep throughout the program, clinicians can make data‑driven adjustments. When planned mindfully, combining exercise with medication supports neural regeneration and long‑term emotional resilience. The goal is balance: using both medicine and movement as equal partners in healing rather than competing approaches.
Caution in Cardiac Conditions
Patients with cardiovascular history must approach exercise for mental health under strict guidance. Anxiety and depression increase sympathetic activity, sometimes overstressing the heart. Gentle aerobic activity such as walking, stationary cycling, or therapeutic yoga proves both safe and effective when performed at moderate intensity. Heart rate monitoring is essential to avoid excess strain. Medical clearance, preferably with a stress test, ensures safety before any endurance or resistance program begins. Temperature, hydration, and medication timing directly affect cardiac response to effort. Exercise should feel comfortable, not competitive. The goal is emotional release, not physical exhaustion. Supervised rehabilitation programs demonstrate significant improvement in mood stability and overall heart resilience, highlighting the delicate balance between psychological healing and cardiovascular safety in clinical practice.
Occupational Anxiety
Work‑related anxiety affects focus, sleep, and motivation—often pushing patients toward burnout. Exercise offers a physiological reset by reducing cortisol and balancing adrenaline. Short, consistent sessions like brisk walking during breaks or post‑work stretching help release tension accumulated throughout the day. Structured programs tailored for professionals especially those in high‑stress environments emphasize mindfulness and gentle aerobic effort rather than exhaustive workouts. Group activities can restore connection and improve empathy among coworkers, lowering emotional isolation. Clinically, regular activity enhances coping ability and expands emotional control under pressure. From a workplace health perspective, it lowers sick days and boosts productivity. When combined with psychotherapy or cognitive training, exercise becomes an anchor that rebuilds both confidence and cognitive stamina in the modern work routine.
quastion of Best Exercises for Depression and Anxiety
What type of exercise works best for anxiety?
Activities that involve rhythm and controlled breathing such as yoga, tai chi, or brisk walking—calm the nervous system and reduce over‑stimulation of stress hormones.
How long should each session last?
Aim for around 30 minutes a day, five times per week. Even shorter bouts, like three 10‑minute walks, can improve focus and emotional balance if done regularly.
What if someone has health issues or takes medication?
They should consult a doctor first. Certain medications affect blood pressure or energy, so exercise intensity and timing must be adjusted safely under medical supervision.
Is there a scientifically recommended weekly plan?
Yes, about 150 minutes of moderate activity or 75 minutes of vigorous exercise per week, combined with rest days and mindful recovery. Consistency matters more than pace or perfection.