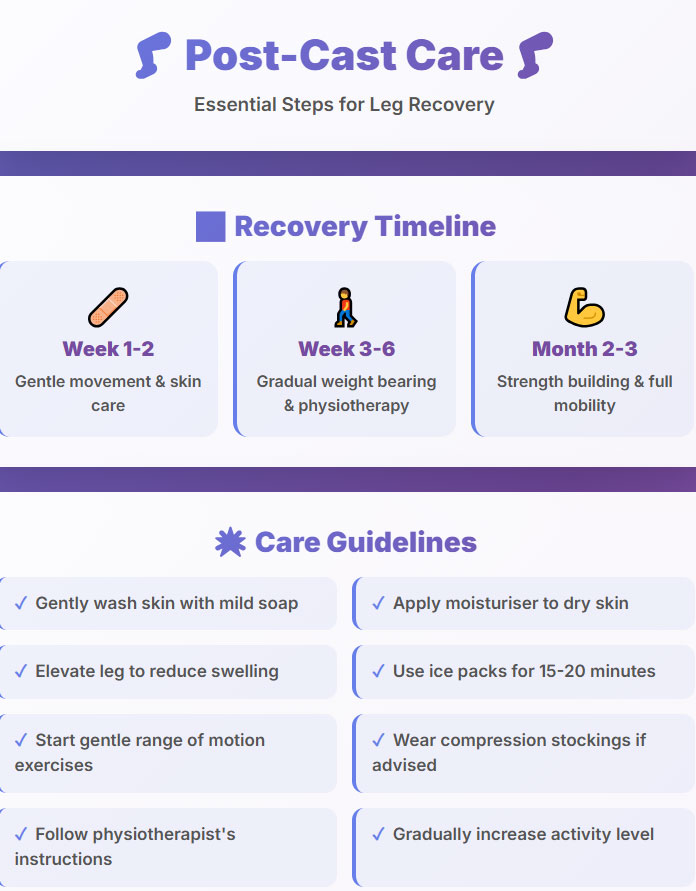
Care after cast removal plays a crucial role in helping the leg regain normal strength, flexibility, and stability after weeks of immobilization. Once the cast comes off, the skin often appears rough or flaky, and the muscles feel noticeably weaker. To restore circulation, warm‑water soaking and gentle massage are recommended daily. Controlled stretching and ankle‑mobility drills gradually enhance coordination and balance, preventing stiffness. Temporary swelling or slight bruising is common and can be managed by elevating the leg and taking short walks as tolerated. Physiotherapy remains a cornerstone of recovery, focusing on movement correction, muscle activation, and posture re‑training. Supportive footwear adds protection and aids proper gait mechanics. Meanwhile, a balanced diet rich in calcium, protein, and magnesium helps bone density improve steadily. With continuous exercise, careful hygiene, and regular professional check‑ups, complete recovery usually occurs within several weeks restoring full comfort and confidence in walking.
WHAT WILL YOU READ…
Natural signs after cast removal
When a cast is finally removed, patients often notice a few natural, harmless changes that might look worrying at first glance. The skin usually appears dry, pale, or slightly scaly because it hasn’t been exposed to air or moisture for weeks. Mild swelling and stiffness around the ankle or foot are common as circulation and joint motion gradually return to normal. Muscles may look thinner due to inactivity a process known as temporary muscle atrophy. Tingling or light pain when moving the limb is also part of early recovery. These conditions are not signs of damage but indicators that the body is reactivating blood flow and muscle function. With gentle massage, short walking sessions, and warm‑water soaking, most of these symptoms fade within days, allowing the patient to regain comfort and confidence in normal movement.
| Stage | Goal | Result |
|---|---|---|
| Skin Care | Re‑hydrate dry skin and restore flexibility | Smooth and soft skin within a few days |
| Muscle Strength | Regain power and joint mobility | Improved strength and controlled movement |
| Swelling Relief | Reduce pressure and discomfort | Noticeable decrease in pain and swelling |
| Mobility Recovery | Rebuild natural walking balance | Confident and stable steps |
| Medical Follow‑Up | Prevent relapse and complications | Safe and complete recovery |
Daily home care
After a leg cast is removed, daily home care plays a crucial role in regaining comfort and preventing complications. The leg has often been inactive for weeks, leaving the skin dry and muscles weak. Establishing a gentle routine helps the limb adapt gradually. Begin each day by moving the ankle slowly to stimulate circulation. Keep the foot clean, dry, and free of excess pressure. Avoid tight socks or shoes that restrict blood flow. Use breathable footwear and rest the leg frequently above heart level. Consistency is key . these small daily steps accelerate healing and reduce stiffness. Recording progress or mild discomfort in a notebook can help track improvement and guide physiotherapy adjustments. Proper daily home care not only speeds recovery but also restores confidence in walking and normal movement after cast removal.
Washing with warm water and using moisturiser
Warm‑water washing is one of the most effective ways to refresh the skin after weeks inside a cast. Use comfortably warm, not hot, water to avoid irritation. Soak the foot or leg for about ten minutes to soften dry layers and loosen dead skin cells naturally. After drying gently with a towel, apply a non‑perfumed moisturiser to rehydrate and protect fragile skin. Avoid strong rubbing or scrubbing, as the skin may be sensitive at first. Regular use of moisturiser improves flexibility, prevents cracking, and restores a healthy tone. For added comfort, do this routine once or twice a day, especially after physiotherapy sessions. Consistent warm‑water care enhances circulation, helps the skin regain elasticity, and prepares the leg for light massage or mobility exercises essential to post‑cast recovery.
Keeping the leg elevated to reduce swelling
Elevation is a simple yet powerful method to control swelling after cast removal. Sitting or lying down with the injured leg raised above heart level promotes proper blood flow and lymphatic drainage, reducing pressure at the ankle and foot. Use pillows or a soft folded blanket under the calf, keeping the leg fully supported without bending it sharply. Avoid standing or sitting for long periods, especially in the first few weeks. Combine elevation with gentle ankle movements to prevent stiffness and improve circulation. This practice not only minimises swelling but also reduces pain and heaviness at the end of the day. Consistent leg elevation, performed several times daily for twenty minutes, accelerates recovery and keeps tissues oxygenated, forming a key part of professional post‑cast home management.

Gentle massage to improve blood flow
Gentle massage after cast removal helps awaken the leg’s circulation system and relieve tension from nearby muscles. Begin by applying a small amount of unscented lotion or natural oil to reduce friction. Using light, upward strokes from the ankle toward the knee improves blood and lymph flow, easing swelling and stiffness. Avoid strong pressure on sensitive or bruised areas to prevent irritation. Short sessions of five to ten minutes, twice a day, can significantly restore mobility and comfort. Massage also stimulates sensory nerves that may have become dull after immobilisation, helping the brain reconnect with normal movement patterns. Combined with stretching and elevation, gentle massage enhances warmth, flexibility, and overall tissue healing a valuable technique every patient can safely practise under physiotherapist guidance during post‑cast recovery.
Stretching after cast removal
Stretching the leg and ankle after cast removal is a key step in restoring full mobility and comfort. When a limb has been immobilised for weeks, tendons and ligaments lose their elasticity, leading to stiffness and reduced range of motion. Gentle stretching helps awaken these soft tissues and improve flexibility without causing strain. Each movement should feel smooth, never forced discomfort is a signal to ease up. Begin with controlled movements, such as rotating the ankle slowly or pointing and flexing the toes. These small, regular stretches improve blood flow, reduce swelling, and prepare the muscles for more active exercises later. Consistency matters more than intensity. Practised two or three times daily, stretching builds the foundation for proper walking mechanics and helps ensure a safe, complete recovery after cast removal.
Gentle ankle stretching
Gentle ankle stretching is often the first type of exercise introduced once the cast comes off. The goal is to re‑educate the ankle joint, allowing it to move freely again after weeks of immobility. Start by sitting comfortably with the leg extended. Slowly move the foot up and down, then make small circular motions in both directions. These simple actions stimulate blood flow, reduce stiffness, and relax the surrounding muscles. The movements should always be pain‑free, focusing on rhythm and control rather than intensity. Gradually, add a towel‑stretch looping a towel around the ball of the foot and pulling gently to feel a mild stretch through the calf. Repeated several times daily, this routine strengthens joint flexibility and prepares the ankle for light weight‑bearing, ensuring a smoother transition back to normal walking.
Strengthening exercises for calf muscles
Strengthening the calf muscles is essential for restoring endurance, balance, and stability after a cast is removed. Prolonged immobility weakens the lower leg, making the first steps unsteady and the joints vulnerable to discomfort. Begin with simple seated calf raises: press the toes downward while keeping the heel on the ground, then lift the heel slowly to engage the whole muscle. Once strength improves, progress to standing raises using a chair for support. Gradual resistance from a stretch band or light weight can further enhance results. These movements activate circulation, support proper posture, and protect against future sprains. Performed regularly, strengthening exercises not only rebuild muscle power but also restore confidence in walking, allowing patients to return to daily activities safely and efficiently after cast removal.

Relearning balance movements
Relearning balance movements after cast removal is a crucial stage in full functional recovery. The brain and body must reconnect after weeks of reduced coordination. Begin with simple tasks like standing on both feet, gradually shifting weight from one leg to the other, and maintaining stability for ten to fifteen seconds. As control improves, progress to single‑leg balance exercises, using a wall or chair for safety. Controlled breathing and focused posture help maintain alignment and prevent falls. These exercises engage deep stabilising muscles in the ankle and core, essential for proper gait restoration. Repetition and patience lead to noticeable progress . smoother walking, improved endurance, and greater confidence. Regular balance retraining not only supports the healing joint but also strengthens neural connections responsible for coordination and injury prevention.
| Week | Activities | Goal | Result |
|---|---|---|---|
| 1 | Ankle rotation, toe flexing | Reduce swelling | Less stiffness |
| 2 | Light stretches, towel stretch | Improve motion | Easier movement |
| 3 | Calf raises, band work | Build strength | Firmer muscles |
| 4 | Balance drills, weight shift | Boost control | Steadier stance |
| 5 | Step‑ups, short walks | Regain confidence | Smoother walking |
| 6 | Dynamic moves, heel‑to‑toe walk | Full recovery | Normal mobility |
Walking correctly after cast removal
Walking after cast removal requires patience and precise technique to prevent strain and speed recovery. The supportive muscles and ligaments are often weak, so body balance must be gradually retrained. Begin by placing the heel first, then roll the foot gently to the toes in a smooth motion. Keep steps short, slow, and even, avoiding sudden twists or uneven surfaces. Using a supportive shoe or a physiotherapist‑recommended brace helps maintain alignment. Focus on posture . shoulders straight, eyes forward, weight evenly distributed on both legs. Combine this with regular stretching and calf strengthening to restore stability and smooth walking rhythm. Practising a few minutes several times a day rebuilds confidence, reduces limping, and ensures safe, natural movement as healing progresses after cast removal.
Step by step Walking correctly after cast removal
Start with posture and balance
Stand upright, keeping your shoulders relaxed and evenly aligned.
Engage your core muscles gently to stabilise your spine.
Place equal weight on both legs before taking the first step.
This forms the foundation for safe, confident walking.
Heel‑to‑toe walking pattern
Touch the ground with your heel first, then roll to the toes.
Push off gently at the end of each step for smooth motion.
Avoid limping or twisting the ankle on uneven surfaces.
This sequence restores joint mobility and natural rhythm.
Controlled short steps
Take small, steady strides instead of long or quick ones.
Keep knees slightly bent to absorb pressure evenly.
Pause and rest if mild fatigue or discomfort appears.
Consistent movement improves strength and confidence.
Support and progression
Wear supportive shoes with flexible, cushioned soles.
Use a brace or walking aid only when medically advised.
Gradually increase step length as pain and swelling fade.
Controlled progress ensures long‑term joint stability.
Physiotherapy after cast removal
Physiotherapy after cast removal is an essential stage in restoring full leg function and reducing long‑term complications. Once the cast is removed, the affected muscles and ligaments are typically weak, stiff, and sensitive. A physiotherapist designs a personalised program to help rebuild strength, restore joint mobility, and improve coordination. Key techniques include controlled stretching, balance re‑education, and gradual weight‑bearing exercises. Each session aims to enhance blood flow, decrease swelling, and relieve discomfort through gentle, targeted movement. Consistency and proper technique are vital to prevent re‑injury. Within a few weeks, most patients regain better range of motion and confidence during walking. Professional physiotherapy not only speeds physical recovery but also helps correct improper movement habits developed during immobilisation, leading to a safer and more balanced return to daily activities.
Evaluation of joint and muscle function
After a period of immobilisation, evaluating joint and muscle function becomes the cornerstone of effective rehabilitation. Physiotherapists begin by assessing movement range, muscle tone, flexibility, and alignment symmetry between both legs. This careful evaluation helps identify weakness, stiffness, or imbalance that must be corrected before active exercise begins. Functional tests such as gait observation and resistance checks reveal how well the muscles coordinate during walking. Detailed measurement of angles and strength levels guides the creation of a tailored therapy plan. Continuous re‑evaluation allows gradual adjustment as the patient recovers. This systematic approach reduces the risk of over‑strain while ensuring steady progress. Proper assessment not only tracks improvement accurately but also prevents chronic movement issues, enabling full and confident use of the leg again after cast removal.
Use of heat therapy and electrical stimulation
Heat therapy and electrical stimulation are two proven physiotherapy methods that accelerate recovery after cast removal. Applying controlled heat improves blood circulation, relaxes tense muscles, and softens stiff tissues around the ankle and calf. Clinical‑grade heating pads or warm compresses are used for several minutes before exercise to prepare the area for safe movement. Electrical stimulation, on the other hand, activates weakened muscle fibres through mild impulses that mimic natural contraction. This process improves strength, enhances nerve response, and reduces post‑immobilisation pain. Both methods complement each other when applied under professional supervision, making exercises more effective and comfortable. Regular use helps patients regain flexibility, reduce discomfort, and rebuild functional muscle control faster, forming an essential part of comprehensive post‑cast physiotherapy treatment.
Specific training for walking without limping
Specific training for walking without limping focuses on restoring a natural, symmetrical gait pattern after weeks of restricted movement. Physiotherapists teach controlled heel‑to‑toe stepping to ensure balanced weight transfer and reduced pressure on the injured side. Strengthening the calf, thigh, and hip muscles builds stability, while targeted stretching improves flexibility in the ankle joint. Balance boards, mirror feedback, and treadmill sessions help correct posture and rhythm with precision. Patients are guided to walk slowly, evenly, and confidently before increasing speed or distance. Attention to proper alignment and muscle engagement prevents compensatory mistakes that cause chronic limping. With consistent practice and guided progression, most individuals regain natural walking ability, improved endurance, and full mobility . completing the final and most rewarding phase of post‑cast rehabilitation.
Treatment of foot swelling after cast removal
Foot swelling after cast removal is a natural response to reduced circulation and muscle inactivity. The treatment focuses on restoring fluid balance, improving blood flow, and rebuilding tissue strength. Elevating the leg several times a day, combined with gentle ankle movement, significantly boosts venous return. Avoid prolonged standing or tight shoes that restrict circulation. Physiotherapists often recommend alternating warm and cold compresses to reduce inflammation. Gentle massage and regular hydration help the lymphatic system clear retained fluids. In some cases, supportive elastic bandages or mild compression socks are advised. Maintaining a balanced diet rich in potassium and low in sodium also supports recovery. With consistent care and proper physiotherapy, post‑cast swelling should diminish gradually over several weeks, allowing the ankle and foot to regain full comfort and mobility.
Lymphatic drainage massage
Lymphatic drainage massage is a specialised, gentle therapy used to relieve swelling after a cast is removed. The technique involves slow, rhythmic strokes that encourage lymph flow toward nearby glands, helping the body naturally drain excess fluids. This massage improves tissue oxygenation, reduces discomfort, and supports faster healing while preventing fluid build‑up. The physiotherapist usually begins near the upper leg before working down toward the ankle to keep the drainage pathway open. Using light pressure is crucial, as deeper force may irritate delicate recovering tissues. When combined with elevation and adequate water intake, lymphatic drainage massage becomes one of the most effective ways to reduce puffiness and restore joint mobility. Consistent sessions promote better circulation, decrease inflammation, and enhance overall comfort during post‑cast rehabilitation.
Alternating warm and cold compress
Alternating warm and cold compress therapy helps control swelling and discomfort after cast removal. Warm compresses increase blood circulation and relax tight muscles, while cold compresses reduce inflammation and numb the painful area. This alternating method trains the blood vessels to expand and contract, strengthening local microcirculation and aiding faster healing. Begin with a cold pack for five minutes, then apply gentle heat for another five, repeating for two or three cycles. Always protect the skin by wrapping compresses in a soft towel. This simple and effective home technique supports other physiotherapy routines by relieving stiffness, easing pain, and encouraging joint flexibility. Used consistently, it accelerates recovery, minimises swelling, and enhances comfort during the transition to normal leg use after cast removal.
Anti‑inflammatory and pain relief medication
Anti‑inflammatory and pain relief medications play a key role in managing swelling and discomfort after cast removal. Non‑steroidal anti‑inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, help reduce both pain and tissue inflammation. These medications support physiotherapy by allowing comfortable movement and improved participation in exercises. Mild pain relievers like acetaminophen can be used when inflammation is minimal but soreness persists. Always take prescribed doses and consult a healthcare professional before combining medications. Proper timing usually after meals reduces stomach irritation. In some cases, topical anti‑inflammatory gels provide localised relief without systemic side effects. Combined with rest, gentle exercise, and hydration, these medicines help restore comfort, promote mobility, and shorten recovery time, leading to a smoother transition back to normal daily activity after cast removal.
Common Questions About Post‑Cast Foot Care
What causes persistent foot stiffness weeks after cast removal?
Persistent stiffness often results from prolonged joint immobility and scar tissue formation. Even after swelling subsides, limited movement can remain until deeper connective tissues regain elasticity through regular stretching and guided physiotherapy.
Can weather changes affect post‑cast foot swelling?
Yes. Cold or humid conditions can temporarily slow lymphatic drainage, increasing mild puffiness. Keeping the leg warm, avoiding sudden temperature shifts, and continuing gentle movement help maintain proper circulation.
How can hydration influence recovery after cast removal?
Staying well hydrated supports the lymphatic system and prevents fluid retention. Dehydration thickens bodily fluids, slowing drainage and healing, while steady water intake promotes faster tissue recovery.
When should residual pain after cast removal be considered abnormal?
If pain intensifies instead of improving, or if redness, heat, or numbness appear around the ankle or calf, it may signal inflammation or circulation issues requiring medical evaluation.
source:
physio-pedia
clevelandclinic